Cytomegalovirus (CMV) in HSCT patients
Cytomegalovirus (CMV) in HSCT patients
Cytomegalovirus (CMV) is a prevalent herpesvirus that is an important cause of morbidity and mortality in immunocompromised patients such as those receiving hematopoietic stem-cell transplantation (HSCT).1
CMV infection is a serious condition for the immune system that can adversely affect transplant outcomes in HSCT patients. The infection can lead to organ toxicity and other complications, including side effects from antiviral therapy, which can further impact clinical outcomes.1
This leads to a higher risk of bacterial and fungal infections. The most frequent clinical manifestations of CMV infection and disease in immunosuppressed patients are pneumonia, enteritis, bone marrow suppression, hepatitis, and retinitis.1
CMV seropositive patients face a substantial mortality disadvantage.2 Possible mechanisms behind this increased mortality include CMV disease (breakthrough; late; drug-resistant), bacterial and fungal infections, sepsis, graft versus host disease (GvHD), and drug toxicity.1
CMV reactivation can occur as early as the day of transplant1
More than 30% of HSCT recipients who were CMV-seropositive or had a seropositive donor experienced a reactivation during their first month post-transplant.1
Cumulative incidence of CMV reactivation in adult HSCT recipients who were CMV-seropositive or had a seropositive donor through 12 months post-transplant
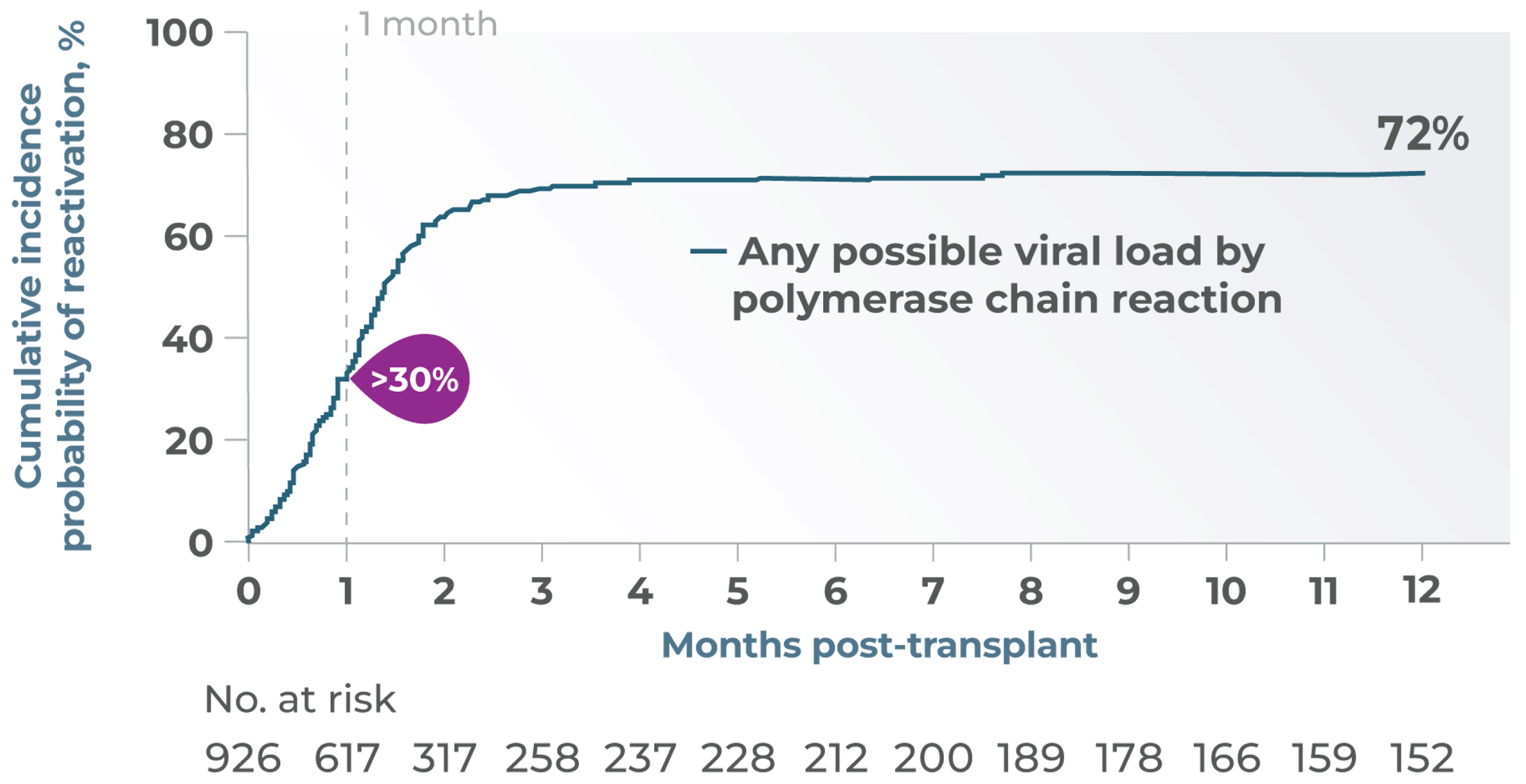
Results from a large period, retrospective, noninterventional cohort study of previously collected CMV viral load data and clinical outcome measures (n=926), conducted at the Fred Hutchinson Cancer Research Center1
References:
- Green ML et al., Cytomegalovirus viral load and mortality after haemopoietic stem cell transplantation in the era of pre-emptive therapy: a retrospective cohort study. Lancet Haematol. 2016 Mar;3(3):e119-27.
- Schmidt-Hieber M et al., CMV serostatus still has an important prognostic impact in de novo acute leukemia patients after allogeneic stem cell transplantation: a report from the Acute Leukemia Working Party of EBMT. Blood. 2013 Nov 7;122(19):3359-64.

