Who are at risk?
Who are at risk?
Several lines of investigation indicate that overall survival is closely tied to the patient’s pretransplant CMV serostatus. Consequently, the primary objective of antiviral supportive care—to lower treatment-related mortality in CMV-seropositive patients to match that of seronegative patients— has remained elusive. The study by Boeckh & Nichols Blood (2004) showcased this impact of pretransplant CMV serostatus on overall survival after allo-HSCT.1
Despite the near-complete elimination of early CMV disease with current strategies, a survival disadvantage persists for high-risk, CMV-seropositive patients (R+) compared with D-/R- patients.
CMV Reactivation
Early CMV Reactivation is Associated with Increased Transplant-Related Mortality and Inferior Overall Survival2
CMV reactivation as a risk factor for nonrelapse mortality and overall survival after allogeneic HSCT (N=9,469)2
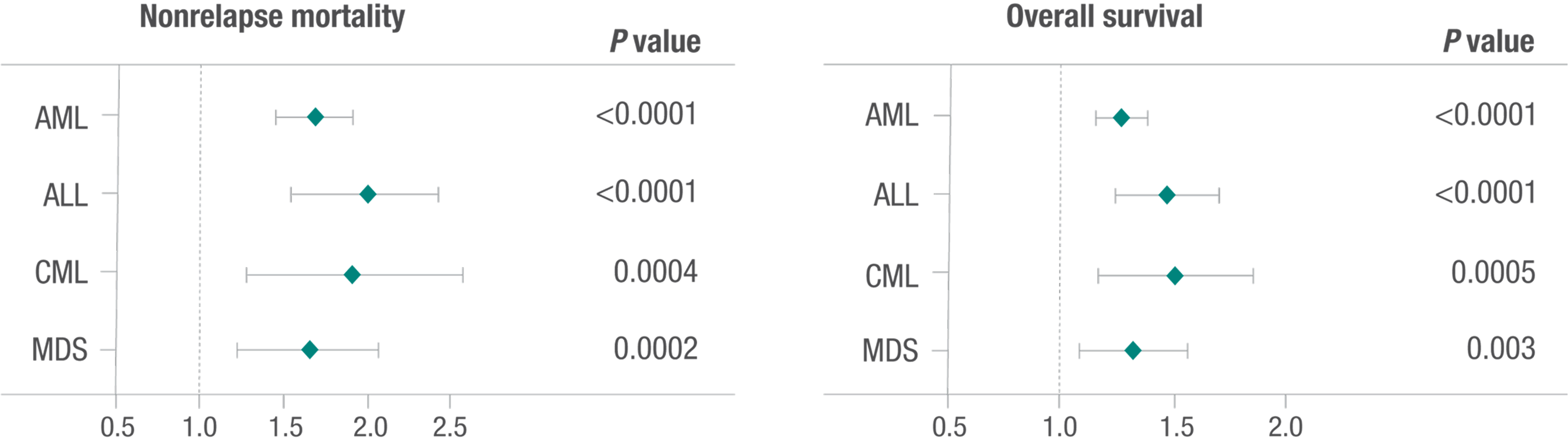
Teira P et al. Blood. 2016;127(20):2427–2438. Adapted from Teira et al.
- A retrospective multivariate analysis of data from the CIBMTR database of first allogeneic HSCT between 2003 and 2010 was conducted to review the impact of CMV serostatus and reactivation on disease relapse, overall survival, and nonrelapse mortality.2
- CMV reactivation was associated with higher nonrelapse mortality, or transplant-related mortality, and lower overall survival among all disease groups: AML, ALL, CML, and MDS.2
- This study observed that CMV reactivation had no preventative effect on hematologic disease relapse, irrespective of diagnosis following initial allogeneic HSCT2
Study Limitations
Limitations of the study: no data were collected on how CMV reactivation was monitored with respect to tests used and values applied for implementing therapy; institutional practices for preemptive and prophylactic therapy vary, affecting the ability to assess efficacy of initial therapy and duration of CMV reactivation; the retrospective nature of the analysis limits generalization of results across transplant settings.
Risk and Burden of CMV
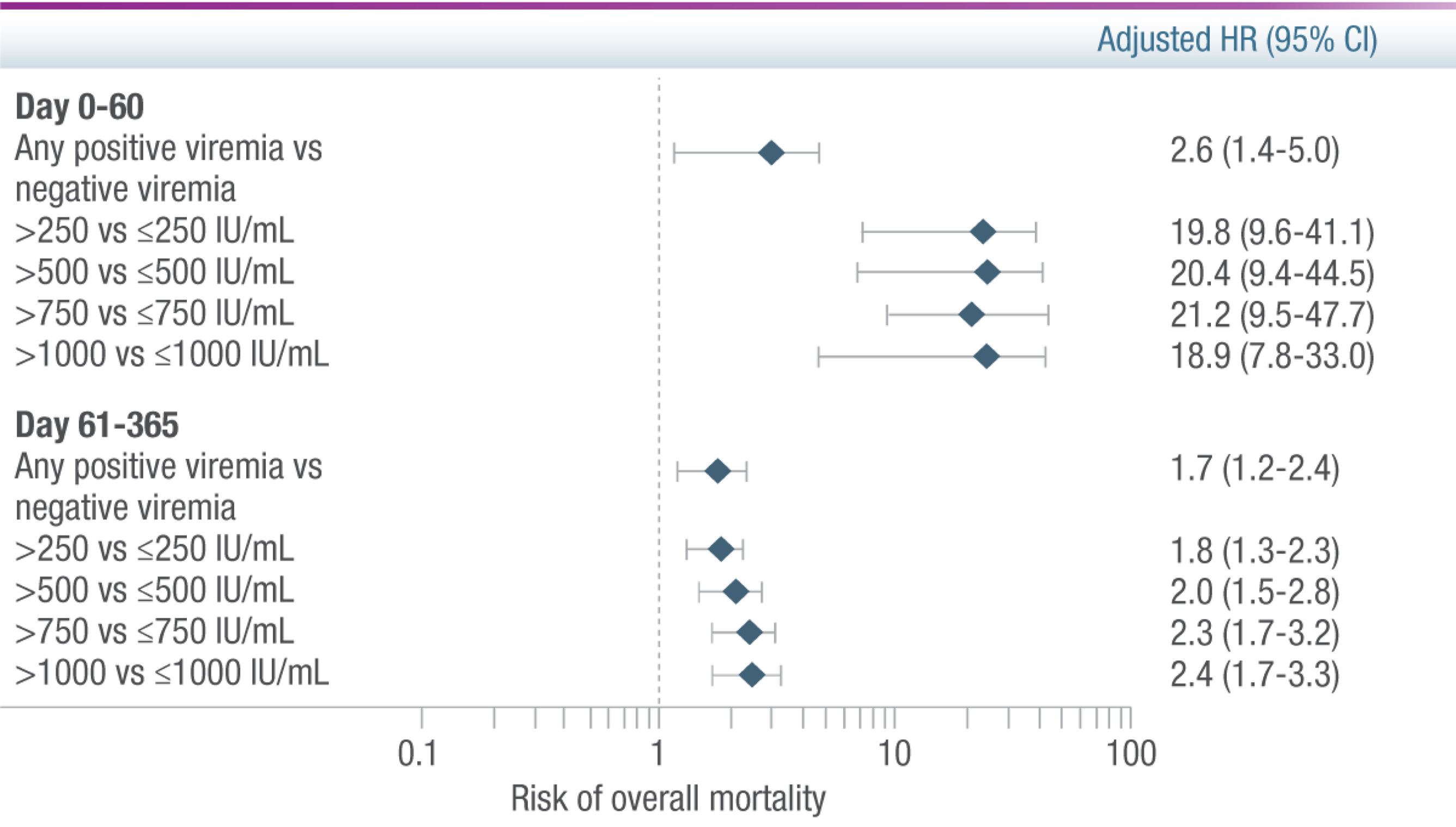
Any positive CMV viremia posed a 2.6x greater risk of mortality in adult HSCT patients compared with patients who had no viremia3
CMV Viral Load as a Time-Dependent Risk Factor for Overall Mortality 1 Year After HSCT (n=926)3
Reprinted with permission from Elsevier.
A large retrospective, noninterventional cohort study of previously collected CMV viral load and clinical outcome measures was conducted at the Fred Hutchinson Cancer Research Center to assess the association of CMV viral load with mortality 1 year post-transplant.3
- Patients were CMV seropositive (R+) or had a seropositive donor (D+)3
- Lowest threshold of 150 IU/mL was used in the evaluation of viremia, as this was roughly the lower limit of quantification for commercially available assays3
Study results:
- Any positive viremia was associated with an increased risk of mortality 1 year post transplant3
- Even adjusting for neutropenia before day 100, the 1-year cumulative overall mortality was 23.1% (95% CI, 20.1–26.1) as observed in the 832 patients who survived to day 1003
CMV viral load is associated with an increased risk of overall mortality in the first year post-transplant3
References:
- Boeckh M, Nichols WG. The impact of cytomegalovirus serostatus of donor and recipient before hematopoietic stem cell transplantation in the era of antiviral prophylaxis and preemptive therapy. Blood. 2004 Mar 15;103(6):2003-8.
- Teira P, Battiwalla M, Ramanathan M, et al. Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: a CIBMTR analysis. Blood. 2016;127(20):2427–2438.
- Green ML, Leisenring W, Xie H, et al. Cytomegalovirus viral load and mortality after haemopoietic stem cell transplantation in the era of pre-emptive therapy: a retrospective cohort study. Lancet Haematol. 2016;3(3):e119- e127. doi: 10.1016/ S2352-3026(15)00289-6

